A group of UChicago researchers recently published a study that found that CBD may help block the COVID-19 virus in mice and human cells. Scientists believe that CBD interacts with the host’s endoplasmic reticulum and interferon signaling pathways in order to block SARS-CoV-2 replication.
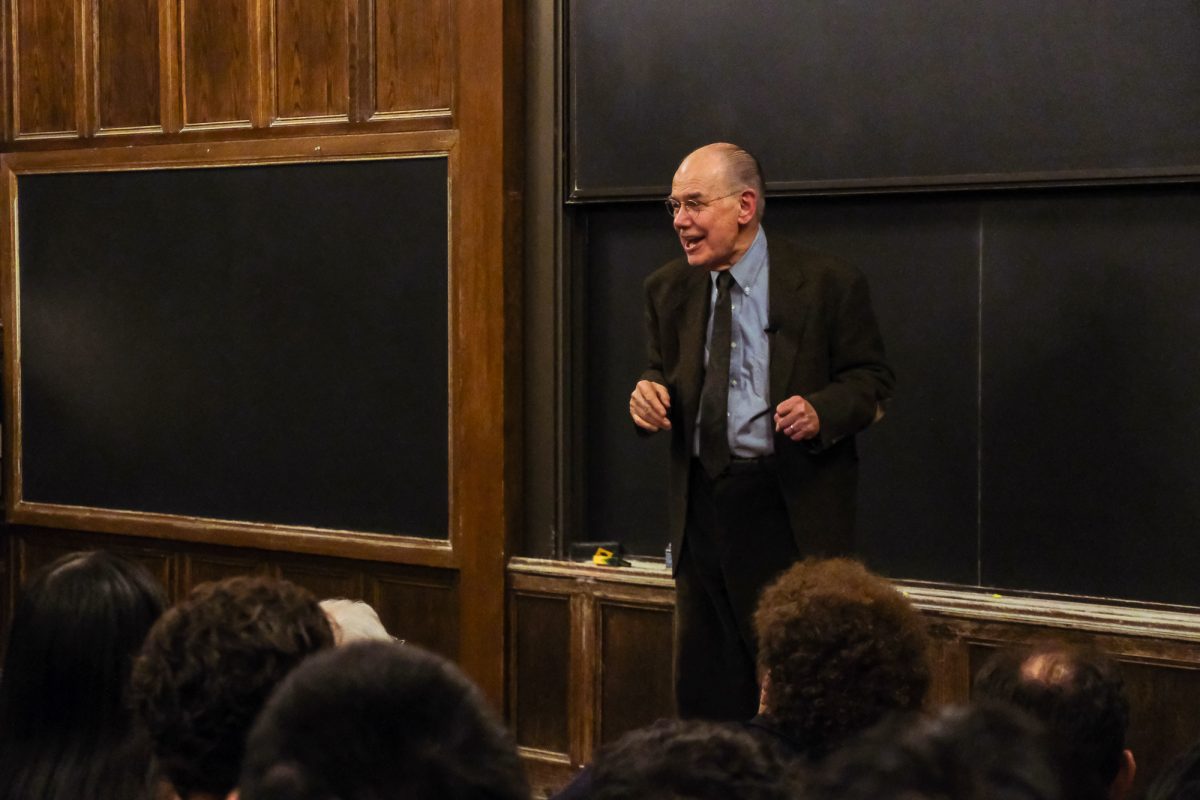
Glenn Randall, one of the authors of the study, is a Professor in the Department of Microbiology. When starting the research process, Randall recalled that the team first brainstormed chemicals that could have anti-SARS properties.
“CBD was suggested because it has anti-inflammatory properties that we thought might dampen a hyperaggressive immune response associated with later stages of COVID-19 disease pathology,” Randall said.
Randall explained that there were a number of surprising results during the study. “The first surprise was that CBD actually directly blocks the ability of SARS-CoV-2 to replicate in lung cells and animal models of COVID. It directly activated genes that our body uses to fight viral infections,” he said. “The second surprise was that patients who were taking an FDA-approved formulation of CBD used to treat epilepsy had significantly less incidence of COVID than similar patients who were not taking CBD.”
In an interview with The Maroon , Randall described his hopes for the researchers’ next steps. “It is impossible to know the value of CBD in treating or preventing COVID without a carefully designed clinical trial. [UChicago researchers] are trying to develop such a trial now.”
Randall also emphasized that the study results should not undermine the current federal guidelines for COVID-19 prevention. “Neither CBD nor marijuana is an accepted preventative for COVID at this time. Vaccines and masking are proven approaches to prevent severe COVID, and CBD should not take their place,” said Randall.
The Maroon also spoke with Dr. Thomas Best of the Center for Health and the Social Sciences about his work for the study. Best echoed Randall’s surprise at their results.
“What was overall surprising to me is that [as] I kept adding more and more controls, or statistical checks and balances, to try to eliminate confounding [evidence]…the association between having a record of CBD and testing positive for COVID was still a significant negative association,” Best said.
Best learned from mistakes with early data, which helped him improve the study’s methods. Prior to working with the National Covid Cohort Collaborative (N3C), Best learned that it’s important, “to be careful about assumptions you make with medical record data. It’s not always clear how different variables are defined, and one needs to be careful and forthright about any assumptions that they made that might be questionable.”
Best also spoke about the interdisciplinary nature of the study. “The number of authors on this is more than I’ve ever been part of, and the depth of work that was done by the collective is more than I’ve ever been part of,” he said. “The different perspectives, the number of different experiments that [were] done, both [with] patients and in cellular analysis, and in mice…. It’s all in one paper.”