University of Chicago Medical Center (UCMC) nurses began taking rotations in the Intensive Care Unit (ICU) on Wednesday, April 15 in order to care for COVID-19 patients, according to ICU-specialist nurses and nurses preparing to return to the unit. As of Monday, April 13, the hospital was treating 125 cases of COVID-19.
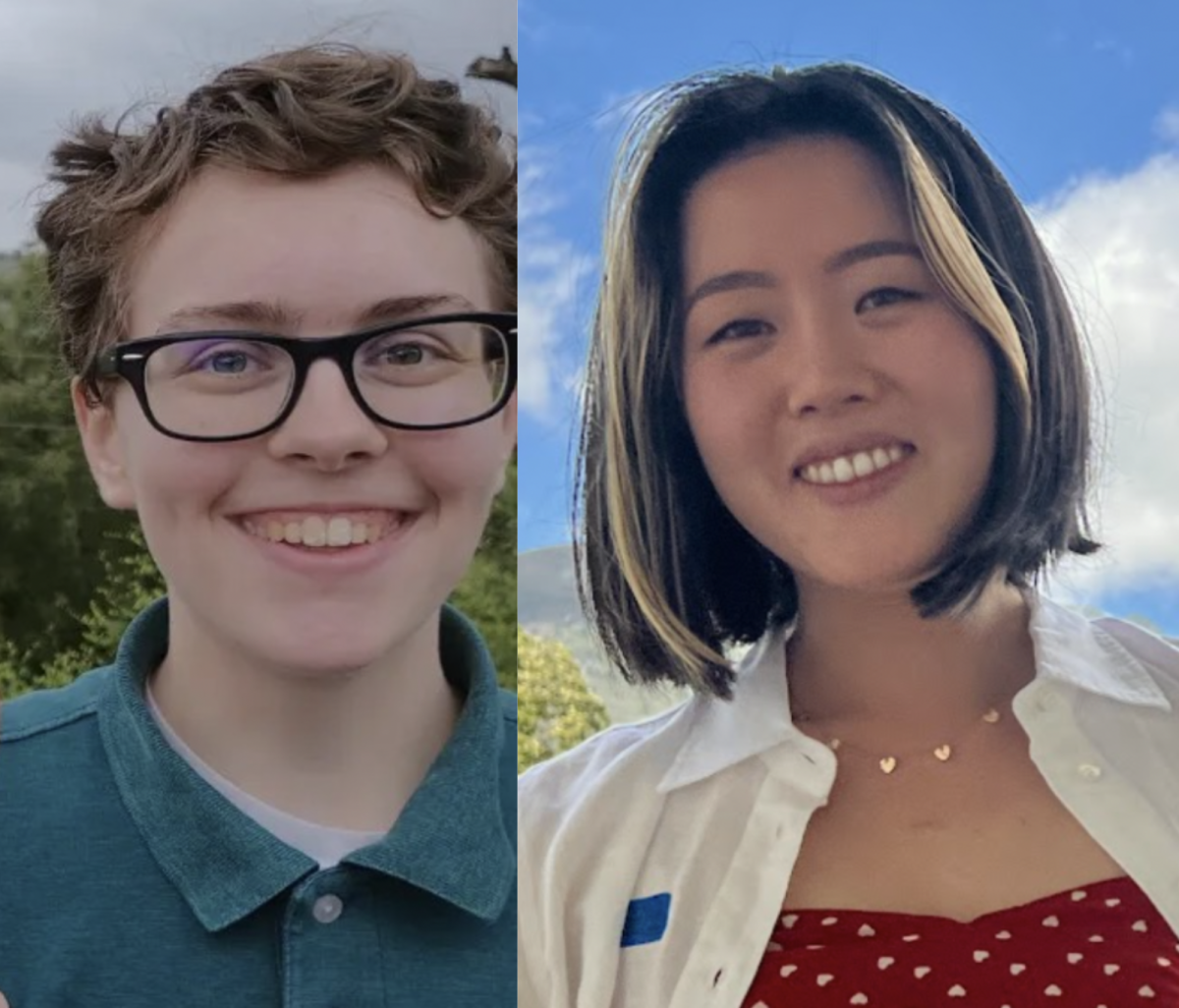
Pamela Valentine, who began treating COVID-19 patients this week, has worked at UCMC for 39 years, most of which she spent as an ICU nurse. Two years ago, Valentine switched to working as a post-anesthesia nurse in the perioperative unit. Now, she’s preparing to jump back into her old role.
“I’m pretty confident with it, but some of the nurses [re-entering] the ICU haven’t had that role for years,” Valentine said. She understood why the change was happening, though, stating “most of the nurses that are currently working in the ICU haven’t had time off.”
Scott Mechanic, currently an ICU nurse, is concerned about the impact the decision might have on patient care.
“The nurses who are rotating in need more training, precepting, support. It’s not that they can’t take care of the patients. It’s that they don’t know where things are, who to call, how to use the technology. And when patients are critically ill, these things can make a difference,” Mechanic said. “While the P.O. [Perioperative] staff do an amazing job, it just doesn’t seem like the best, safest care for our patients.”
Mechanic works in a 24-bed ICU unit that has been converted to solely treat COVID-19 patients. He added that non-medical staff is currently strained as well—a lack of manpower which has created problems maintaining units. Aside from medical attention, cleaning and maintenance services are essential to keeping ICUs functional.
“Where the hospital is really lacking support is with environmental services…and lower wage ancillary staff. They have not gotten training. Units aren’t being cleaned. Equipment isn’t getting brought to the unit,” he said.
According to Mechanic, UCMC is “mostly full, not completely full of COVID-19 patients”. The vast majority of people being treated are Black—which he noted is not a huge change from ordinary times, but also fits the disproportionate impact of COVID-19 on Black Chicagoans overall. Despite making up 14.5 percent of the population, Black Chicagoans account for 27.5 percent of COVID-19 cases and 43.5 percent of deaths.
Mechanic and Valentine both work in close proximity to the virus and have taken precautions to protect themselves against infection. However, Mechanic said that although he’s taking the steps to prevent himself from catching the virus, he is more concerned about the negative impact the infection could have on those around him.
“I’m worried that if I get sick I’ll spread it to other healthcare staff and other people in my life. I’m more worried that I won’t have the opportunity to provide the best care possible to my patients,” he said.
Valentine is wearing a mask and gloves at all times. “I feel safe because I am taking care of the things I need to take care of,” she said. “But you don’t know who has it and who doesn’t. It’s definitely a concern.”
UCMC has recently begun accepting transfer patients from other area hospitals, although Mechanic worries the hospital could be doing more to assist those with heavier caseloads.
Valentine noted, “we’re not yet overwhelmed yet. But we haven’t met the curve.”