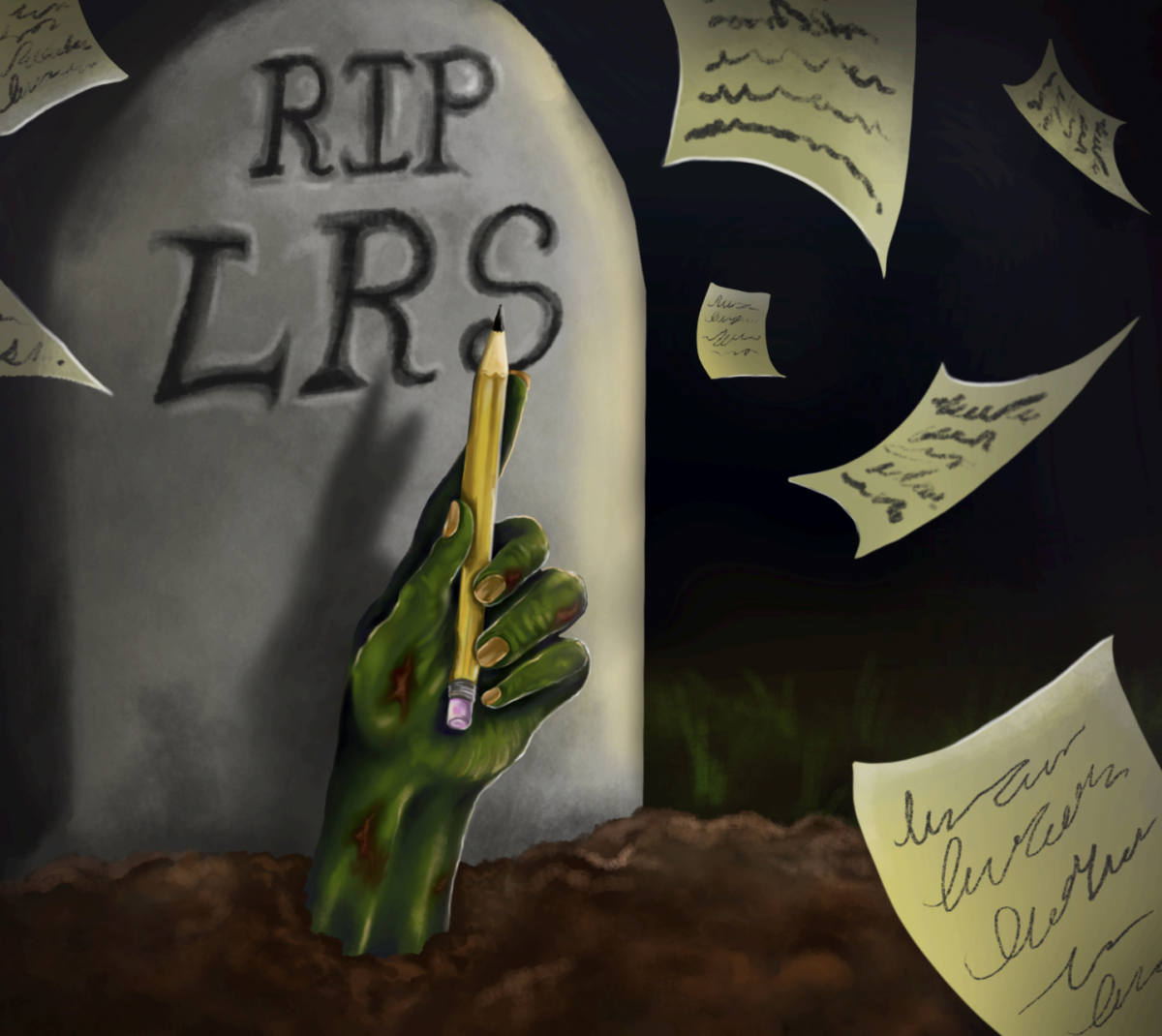
The recent layoff of 450 employees at the University of Chicago Medical Center (UCMC) has caused a great deal of concern and consternation. Workers and their supporters are protesting this drastic action, while community leaders and campus activists are raising a hue and cry to call attention to it. This event is likely to amplify the already strained relations between the community and the Medical Center, and magnify the scrutiny with which its programs and policies have been evaluated.
The trouble with UCMC’s decision is not just a matter of jobs lost, although the personal and community-wide impacts are doubtless very distressing. It is understandable that cuts will be made on account of budget shortfalls, but it is not entirely defensible, given the possibilities for slashing costs in other areas or implementing furloughs. For those unfortunate workers turned out of their livelihoods last week, it must be especially hard to watch an expensive new medical pavilion go up next door as their own incomes disappears.
But the big trouble with UCMC’s decision is that it heats up some issues that have been stewing for years without anybody to cool them off. There’s a looming question as to what priorities the Medical Center holds (and actually practices), and how compatible they are with community needs and expectations. Critics view last week’s layoffs as a strategic move to discard those personnel associated with hospital functions slated for radical reductions or restructuring. Indeed, UCMC’s staff reduction coincides with the introduction of a new emergency-room triage system by dint of which patients not in need of critical care—however defined—will be turned away.
In a way, this two-part maneuver seems less like a reluctant and unpremeditated response to the fickleness of finance and more like the culmination of a journey whose trajectory was set long ago. While UCMC’s rhetoric certainly hasn’t coupled the change in policy with the cuts in staff, cost savings enjoined on both accounts announces loudly and clearly what are the priorities of the future, and what are the practices of the past.
UCMC bills itself as a teaching and research hospital and emphasizes the specialized nature of the medicine relevant to that mission. Not only is it unsuited to delivering general care, but also the costs of doing so are apparently greater—up to 60 percent—than for other hospitals.
Yet UCMC retains special status as a non-profit hospital, enjoying exemptions from income, property, and sales tax and the benefit of issuing tax-exempt bonds to raise capital. Commensurate with those privileges, UCMC is supposed to provide charitable services to the public.
The contention is that UCMC is reneging on its obligation to provide charity care by putting a lock on its doors for those needing general care, cutting its capacity to serve poor and uninsured residents. An extensive program called the Urban Health Initiative now serves as the masthead for the current orientation to local public health policy. Until recently, one component of the program was to provide patients with the option of being redirected and shuttled from UCMC to participating community health clinics. Now, with a firm step forward, the “optional” part of that program has ended—it will be mandated.
In considering the misapprehension of patient ailments that often leads to adverse circumstances when patients are turned away for wont of “critical” conditions by hospital staff, UCMC’s program is bound to warrant more than a little concern. One wonders where to draw the line on “critical,” and if the line will be drawn without prejudice to those whom, according to its critics, the policy seems most directed—those without coverage. Indeed, the American College of Emergency Physicians recently condemned UCMC for “patient dumping,” and described its strategy to “cherry pick” patients as a dangerous precedent.
UCMC notes that the gist of its program is to streamline patient care, and it is beyond dispute that serving residents with preventative and regular care at a primary care home, thereby eliminating unnecessary calls to the E.R., is a sound idea.
The issue is that UCMC’s practice of incubating community health centers seems geared not simply toward rationalizing and improving health services on the South Side, but financially and morally divesting from them as well. For UCMC, relocating patients to health centers eligible for state and federal funding streams is a means of keeping its own purse strings closed, and concentrating instead on the things it most cares about: teaching and research.
Both UCMC and its critics have valid arguments to make, but in the last analysis, the onus is on the hospital to make clear how it provides the services required of its non-profit status. As access to healthcare continues to field incredible national interest and concern, UCMC will have to assert what role it will take in the future, and clear up the stains on its public persona.
Marshall Knudson is a third-year in the College majoring in anthropology.