Researchers at the Institute for Molecular Engineering at UChicago have discovered a new malaria vaccine system that may be more effective than the existing vaccine.
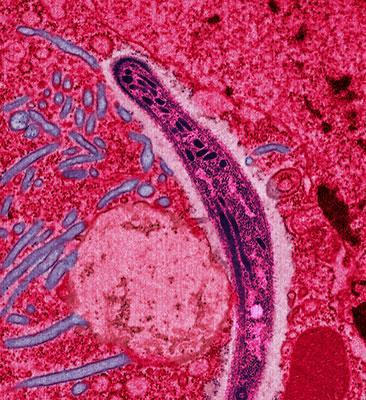
According to the Center for Disease Control, malaria is a disease caused by a parasite, *Plasmodium falciparum*, that is transferred from mosquitos. In 2016, malaria resulted in 445,000 deaths out of 216 million diagnoses worldwide. In the United States, there are about 1,700 cases of malaria each year.
The World Health Organization says that the preexisting malaria vaccine RTS,S/AS01 can protect children at phase three of malaria, but its effectiveness tends to be limited to 30–40 percent of patients.
The new malaria vaccine system involves a subunit vaccine that uses antigens, or proteins derived from a pathogen (the bacteria causing the disease), and adjuvants, agents that further enhance immune response to antigens.
Malaria vaccines have to secure protection from pathogens and eliminate already infected cells. There should be a localized delivery of adjuvants, resulting in inflammation of only specified targets.
To fulfill such criteria, a new vaccine system targets specific cells in the immune system using polymeric glyco-adjuvant conjugated with an antigen. “Polymeric glyco-adjuvant” comes from combining “polymer,” a series of similar molecular units chained together, and “glyco,” which means sugar.
Viruses and bacteria have sugars on their surface, while the dendritic cells in our immune systems have sugar-specific receptors. In the presence of sugar, dendritic cells activate T cells, heightening immune response. The adjuvant in the new vaccine is mediated with mannose, a type of sugar. Therefore, the vaccine can aim at dendritic cells to activate pathogen-specific T cells.
This method encourages greater T-cell response, making it more promising than previous vaccines. These T cells also help clear infected cells, while current vaccines’ mechanisms cannot.
“This work could potentially have applications in vaccinations against complex infections and cancers,” says UChicago professor Jeffrey Hubbell.
UChicago faculty members are collaborating with Emory University on further research to determine if this kind of vaccine can be used to treat other diseases.
Further information on this scientific discovery can be found in Nature Materials.