This year marks the fifth anniversary of the University of Chicago Medicine’s Level 1 Trauma Center. To commemorate this milestone, The Maroon spoke to Dr. Selwyn Rogers, founding director of the Trauma Center, and local nonprofit leaders Paul Robinson and Teny Gross about what the Center has accomplished within the community and its goals for the future.
Since its establishment, the adult trauma team has treated 18,494 adult patients, and its pediatric trauma team has cared for 2,893 children. The Center’s violence recovery team has also helped 7,761 people transition back into the community through social and behavioral health agencies to reduce the risk of re-injury.
The Trauma Center and its benefits did not come to UChicago easily; the South Side community campaigned for the creation of a trauma center for years before plans to establish the UChicago Trauma Center were unveiled in 2015.
Community demand for a local trauma center came after a 1984 protocol change mandating that emergency medical services transport the most severely injured patients to the nearest trauma center instead of the nearest hospital. The amendment was the result of the death of Benjamin Wilson, a top-ranked high school basketball player who was killed at the age of 17 by a gunshot wound. Wilson was taken to nearby St. Bernard hospital to treat his injuries but had to wait almost two hours for treatment.
The rule change left patients in the South Side, which did not have a trauma center, without access to local treatment for severe traumatic injuries for the next 27 years, leading to the deaths of many more civilians. Among them was Damian Turner, an 18-year-old community activist who was shot on August 15, 2010, blocks away from UChicago. Turner died because there was no adult trauma center nearby that could treat his injury. His death raised the first calls for the establishment of a trauma center at the University.
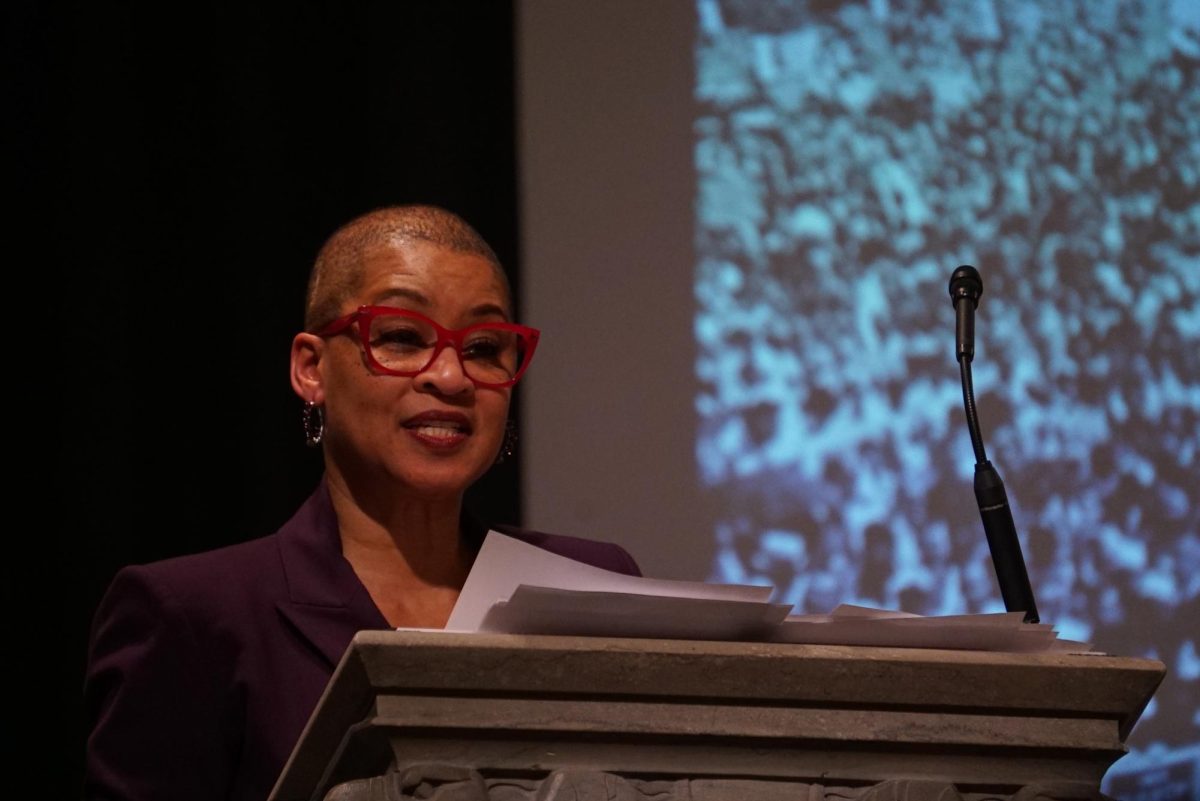
“[Many community groups] rallied around the idea that a trauma center needed to exist on the South Side, and the most logical place for that was the University of Chicago, the only academic center on the South Side of Chicago,” said Trauma Center Director Dr. Selwyn Rogers. “That resistance lasted six years before the University of Chicago changed their minds.”
“The opening up of a Level 1 trauma center at UChicago Medicine, which hadn’t been present for almost three decades, was a pivot, symbolic and literal, of the University of Chicago Medicine toward the community instead of away from the community,” Rogers added. “The community has always believed that they needed and deserved the Trauma Center. The university denied that belief.”
As a non-native to the Chicago area, Rogers reports having faced backlash from members of the surrounding communities when he was first recruited to lead the Trauma Center.
“I’m an outsider,” Rogers said. “[The community] didn’t see Selwyn Rogers, a trauma surgeon building a trauma center. They saw UChicago, a place that has not been friendly to them.”
Rogers stated that many community members lacked faith that UChicago’s Trauma Center would be here to stay, adding that one of the most important parts of the Center is that it strengthens trust with the community.
“[The Center] is successful,” Rogers said. “It’s not going away. It’s fully embedded now. It’s part of the DNA of the institution.”
Over the past five years, the Trauma Center has also partnered with several nonviolence-advocating community organizations to enhance the Center’s care and help them mitigate the effects of gun violence at every step, including prevention, care, and recovery.
For example, their violence recovery team works closely with Chicago Create Real Economic Destiny (CRED), a local nonprofit for gun violence prevention. CRED’s Deputy Head of Programs, Paul Robinson, explains that they assist with patients’ legal issues and “connect the dots” necessary to help them “return home,” emphasizing the importance of personalized care.
“[Recovery] takes that kind of collaborative and really personal touch of relationship building. From the hospital to community-based organizations to make sure that we’re having a holistic response.”
To further this type of holistic care, the Trauma Center also works closely with the Institute for Nonviolence Chicago to focus on the mental health aspects of recovery. Founder Teny Gross highlights the need for consistent follow-ups, particularly with trauma patients.
“[Even those who are] completely innocent and are not caught in the cycle of [violence], they don’t go back to normal,” Gross said. “They’re not the same after they were shot, even if they had nothing to do with street life…people lose their jobs, get depressed, their families fall apart, so investing in support is really important.”
Rogers also emphasized the psychological impact of trauma on patients, noting a general lack of focus on this subject.
“The mind is actually pretty challenging to figure out how best to repair because it’s not completely clear. To some people, it’s faith. For some people, it’s therapies…But there’s no individualized plan,” Rogers said. “And I can’t ignore the fact that providers, nurses, doctors, residents, medical students are also traumatized by seeing traumatic things.”
Currently, there is no dedicated center that addresses this psychological impact. “It is a huge problem in this country,” Rogers said.
Though Rogers noted areas where the Trauma Center can improve, Gross and other community members highlighted the distinctive approach taken by the Center’s team.
“There’s a strong emphasis at the Trauma Center at UChicago on the humanity of how people are received and treated—the respect,” Gross said. “It’s not just how we’re able to patch your blood vessel…It is how we treat it, right? Are we treating you as a full human being? We see potential and we see love in you. So I think that the University of Chicago Trauma Center has built a model that can really spread to other places.”