“Is my jaw broken?” I wondered frantically as I picked myself up off the black ice on 59th Street. Gingerly pressing my chin left a reddish stain on my glove. “Is this going to need stitches!?”
After I tumbled from my bike one recent Sunday morning, the only nearby soul to answer these questions was a UCPD officer. “I’m not an expert,” he mumbled apologetically, taking a look. “Maybe go to the emergency room if you got time, but it looks like you’ve just got a scrape.” That description sounded like something a dining hall first aid kit could handle, but I quickly learned otherwise.
“We don’t have any spray,” the Aramark employee said, rummaging through Cathey’s first-aid kit. They did, however, have a pair of bright blue band-aids for my chin.
Within walking distance of Chicago’s premier research hospital, I carefully pedaled back to my dorm, where I had my own tube of Neosporin.
Some of the University’s medical shortcomings are old news to readers of the Maroon. Back in November, Students for Health Equity (SHE) made headlines when it delivered a pair of coffins to the University of Chicago Medical Center’s front door—the latest in what the group’s Facebook page calls “a combination of educational events and direct-action protests to encourage the University of Chicago Medical Center to open an adult level-one trauma center.” A worthy goal, but also the only goal mentioned on SHE’s website, despite the group’s stated mission to “address health disparities on the South Side.” As I learned during my misadventure last Sunday, “health disparities” don’t only affect life-or-death emergencies.
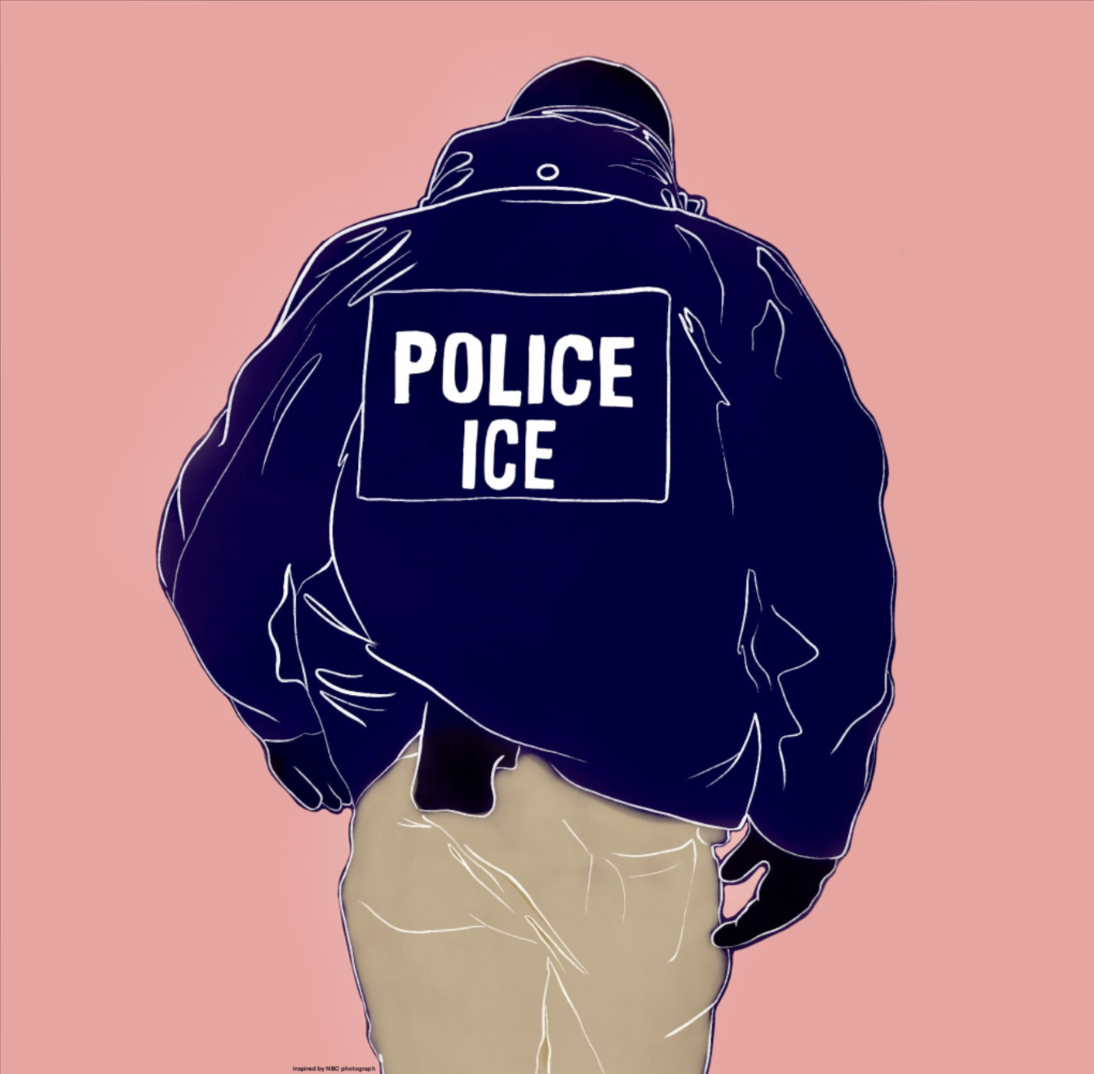
The vast majority of the students who march with SHE—or the residents they march for—will never fly through a windshield or suffer multiple gunshot wounds. They will, however, have plenty of slips and scrapes like mine on Hyde Park’s icy streets. The University of Chicago Police Department’s (UCPD) officers are a familiar presence on many of those streets, but as I learned the hard way last Sunday, they can’t provide so much as a band-aid. The UCPD might not save any lives by installing first aid kits in its squad cars. It will, however, be able to treat the cuts and bruises of students and South Side residents alike. It might also begin to heal years of sore feelings between South Side and the UCPD.
What about social justice? Doesn’t UChicago have an obligation to bring trauma care to a violent part of one of America’s most violent cities? In fixating on that argument, SHE seems to have overlooked other, more mundane inequities. During my unplanned investigative-reporting trip to the dining hall, I learned that the men and women who spend hours each day among sharp knives and open flames don’t have access to antiseptic spray. Nor do they have the luxury, as I did, of going off-site to properly treat a cut. Bringing dining halls’ first-aid kits up to OSHA standards won’t make for a dramatic photo op. It will, however, save time and dexterity lost to infections and minimize the chance that blood or pus will find its way into your scrambled eggs. Who knows? It may also boost Aramark’s chances of actually passing its health inspections next year.
None of these goals have the same panache as building a multimillion-dollar facility and alleviating a gross health-care inequality in America’s third-largest city. Even so, might SHE accept them as smaller, more pragmatic steps for its namesake mission? First-year SHE member Daphne McKee voiced cautious support. “The members of SHE individually would most likely all be supportive of any other smaller efforts to improve health equity in the region,” she explained. “If there were smaller and more short-term campaigns that could improve health care in the region, and could get us visibility for the trauma center campaign, and that we could undertake at the same time as the trauma center campaign, we would probably be up for it” (emphasis hers).
Would a few afternoons’ worth of fundraising be “short-term” enough? Buying 100 of Quake Care’s OSHA-compliant first-aid kits—for installation in UCPD cars, dining halls, and elsewhere around campus—would cost $2,495. Contrast that amount with the UCMC’s current $737-million debt, and the nearly $6 million in today’s dollars that it lost while running a trauma center from 1986 to 1988.
Which leaves me with a question for SHE’s econ majors: In the near term, which do you think is more likely to get a check?
Patrick Reilly is a first-year in the College.